Cementless by Dr.Thomas Gross
New paper by Thomas Gross 1/11/2011
WHAT IS THE BEST BONE FIXATION TYPE?
A Comparison of cement vs. bone ingrowth
Thomas P. Gross, M.D.
- At 2 years of follow-up cemented and uncemented femoral resurfacing is equivalent.
- Femoral cement failure is the most common late cause of failure in hip resurfacing (3% @ 8 years).
- Wear-related failures with the Corin or Biomet implant systems are rare in my experience.
- We have demonstrated that failure of bone ingrowth does not occur in a properly designed uncemented femoral resurfacing component (provided femoral neck fracture or osteonecrosis does not occur).
- Uncemented fixation of implants in stemmed total hip replacement surgery is more durable at 10 years than cement, especially in young active patients.
- Every patient who is a candidate for hip resurfacing is a candidate for an uncemented femoral resurfacing component.
Most clinical data on hip surfacing to date is based on an uncemented acetabular component and a cemented femoral component.
- Uncemented femoral resurfacing components are now available from Biomet for any patient who desires them.
- Wright Medical is beginning initial studies on an uncemented femoral component.
- Corin has had an uncemented femoral component available in Europe for several years.
- I recommend uncemented resurfacing for every patient who is a resurfacing candidate; I don’t require cemented components or stemmed total hips as backups except in unusual circumstances (2/2300 = 0.23%).
- Combination of the Biomet Magnum and Recap components for total hip resurfacing is defined by the FDA as an off-label use.
I recommend uncemented fixation of both the femoral and acetabular components of metal-on-metal hip resurfacing devices. Currently, the market standard used by most surgeons around the world is uncemented fixation of the acetabular component and cement fixation of the femoral component. I was one of the first surgeons in America to begin performing metal-on-metal hip resurfacing in 1999. I was the first to begin resurfacing with a fully porous coated uncemented femoral component that I developed with BIOMET in 3/2007. I currently lead the world in uncemented metal-on-metal hip resurfacing with over 1300 operations performed. The initial results are excellent and other companies are beginning to explore this technology as well. The speed of recovery is no different than if a cemented femoral component is used. The early results are the same. I believe (but have not proven) that the long-term fixation will be superior. Let me explain why.
Uncemented femoral components for metal on metal total hip resurfacing have shown excellent results during the initial 4 years that I have been using this new technology. The early results that I have achieved in over 1300 cases since March 2007 are better than the early results that I achieved with the same brand cemented femoral component. But this may simply be due to greater surgical experience. In a comparison study to be published in Orthopedic Clinics of North America in April 2011, we found no difference in the results of matched patient groups with either cemented or uncemented femoral components implanted during the same time period at early (2 year) follow-up. All uncemented femoral components were found to be bone ingrown by XR criteria. This means that the attachment of these uncemented femoral components is highly successful. My opinion is that they will therefore outlast cemented components in the long run. We will provide a detailed summary of the results of this study as well as the latest results in the first 1000 uncemented hip resurfacings.
Uncemented fixation of implants to bone is a proven technology that has generally surpassed the durability of cemented fixation to bone in traditional stemmed total hip replacement surgery. In the long term (at 10 years) a higher percentage of hip implants using uncemented fixation still remain attached to the bone than cemented implants, especially in younger more active patients.
Fixation of total hip implants to bone can be accomplished by cement or by porous ingrowth technology (uncemented). Cement fixation is immediate. Cement is an acrylic material (methylmethacrylate) that is very brittle and also fairly toxic to bone cells. Cemented implants gradually loosen from the bone over time by reaction to the cement itself and due to gradual fatigue failure of this material. This process is faster in more active patients and faster in implant situations where the cement is stressed by shear forces rather than by compression forces.
Uncemented components are initially held to the bone by a very tight press fit, which is achieved by accurately preparing the bone so that the implant can be tightly hammered-on. The implants are so tightly wedged–on that the patient can bear full weight on them immediately. They do require a period of six to twelve months of bone ingrowth before they are considered well fixed. There is usually a small chance of failure of this bone ingrowth process in uncemented implants (<1%). But if ingrowth occurs, it is much more durable than cemented fixation and rarely fails in the long term.
Because orthopedic surgeons in America have come to a consensus on the superiority of uncemented fixation in total hips, uncemented fixation has virtually completely replaced cemented fixation in stemmed total hip replacements, despite the fact that these implants are more expensive. 99% of acetabular (socket) components that are used today are of the uncemented type, as are about 90% of femoral stems. In hip resurfacing there is also universal agreement that uncemented fixation is superior for the acetabular component. However, until recently, uncemented femoral components have not been available, therefore most hip resurfacing operations in the past have employed cemented fixation of the femoral component.
At the time that I began hip resurfacing in 1999, there was not yet general agreement that uncemented fixation was superior to cement in hip replacements. However, the evidence was mounting that uncemented fixation was better. I therefore did not think it was logical to use cemented fixation in hip resurfacing, an operation developed specifically with the more active younger patient in mind. The only companies pursuing hip resurfacing at the time were two small English companies: Corin and Midland Medical Technology (maker of the Birmingham implant). I suspect that they did not have the financial resources to develop a more complicated uncemented femoral component. I began working with Corin 12 years ago, but they were unable to manufacture a porous coated femoral component at that time. I therefore worked with Biomet on an uncemented femoral component and the precision instrumentation required for this implant for five years. I first began implanting it in March 2007. The Biomet component has a full coating of Titanium plasma spray under the entire under-surface of the femoral component. Recently they have added an additional layer of hydroxylappatite (HA) to increase the speed and extent of bone ingrowth. This is the best implant available to maximize the chance of bone ingrowth.
When I started working with Biomet to develop an uncemented femoral component, Corin also started to work on one. They were able to bring it to market in Europe first; however, their component is only partially porous-coated (less than 50%) with Titanium (but it does have complete hydroxyl appetite coating). I personally do not believe this is good enough for long-term fixation (>10years), but nobody knows for sure yet. It is not yet available in the US.
There have been limited trials of uncemented femoral components in resurfacing in the past. Most of these did not have adequate porous surfaces for ingrowth fixation. This was true, for example, for the early uncemented femoral McMinn device which was abandoned.
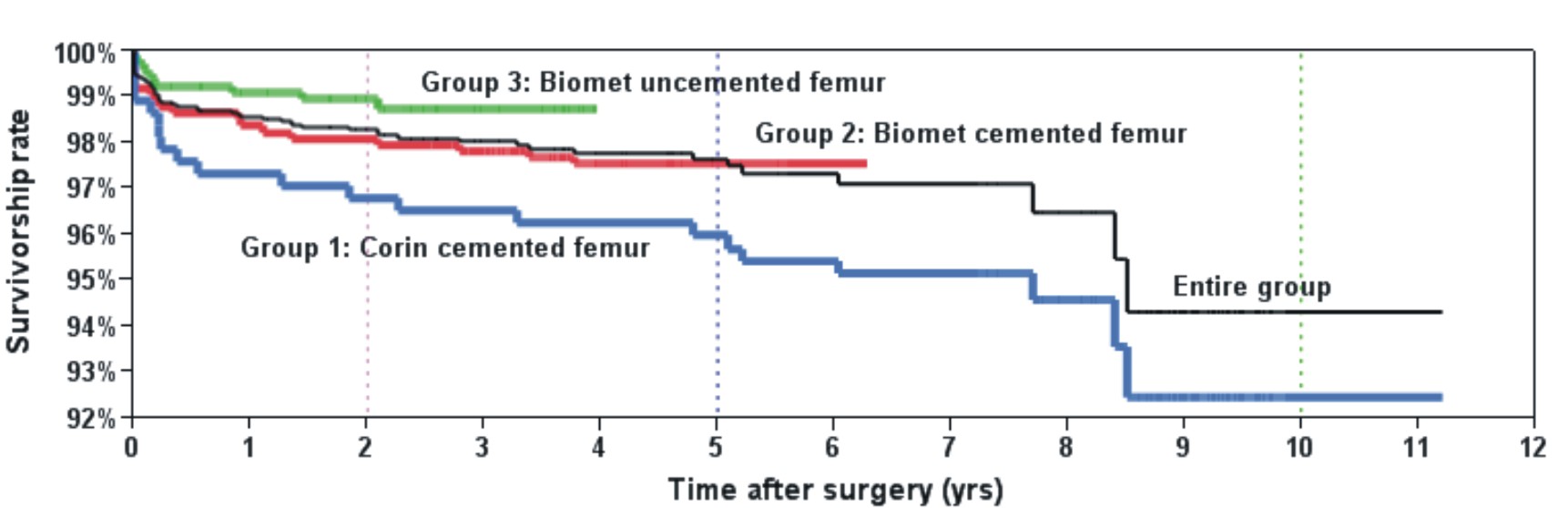
Theoretically, cement is the weak link when long-term (> 10 years) fixation of the femoral component is contemplated. I have found this to be true when evaluating my 5-8 year results with the Corin system. In 2001 I started the US FDA study that led to the approval of the Corin resurfacing device in this country. My success rate at the 8-year mark is 94% in 373 cases. Half of all failures, at 3%, are due to loosening of the cemented femoral component. In my experience, this has been the primary cause of failure overall, and the most common source of late failure. Recently, there have been some reports of wear-related failures from the Oxford Group and others; in the Corin study, I had only 0.5% failures due to this problem (for a detailed discussion of this topic, please see my article on “wear”)
TABLE 1: COMPARISON STUDY (computer matched groups)


Uncemented Group Cemented Group
Number of cases: 191 96
Avg. Follow-up: 2 years 2 years
Harris Score: 94± 10 96±6
UCLA Activity Score: 8 ±2 7 ±2
All Failures: 2% 2%
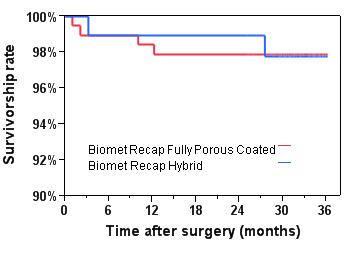
TABLE 2: FIRST 1000 BIOMET UNCEMENTED HIP RESURFACINGS:
Follow-up: Average: 18 months // Minimum 2 years: 46%
Survivorship: 98.5% at 3 years
Harris Hip score: 95 + 8 after 2 years
UCLA Activity score: 8±2
Failures resulting in revision surgery:
1. Femoral neck fractures: 6 (0.6%)
2. Femoral head osteonecrosis: 2 (0.2%)
3.Acetabular failure of ingrowth: 3 (0.3%)
Other Significant Complications:
1. Deep infections: 3 (0.3%)
2. DVT (blood clots in the leg): 2 (0.2%)
3. PE (blood clots in the lung): 2 (0.2%)
4. Dislocations (isolated 1 time): 2 (0.2%)
There were none of the following complications in the first 1000 cases:
1. Nerve injuries
2. Blood transfusions
3. Loose femoral components after 1 year (either by XR or otherwise)
4. Adverse wear problems (“pseudotumors”)
5. Implant revision due to infection
6. Implant revision due to recurrent dislocation.
7. Other significant medical complications
8. Death
FIGURE 2: SURVIVORSHIP CURVES OF DR. GROSS’ HIP RESURFACING GROUPS:
Group 1: Corin cemented femur: 2001- 2005 #373 cases
Group 2: Biomet cemented femur: 2005- 2008 #740 cases
Group 3: Biomet uncemented femur: 2007- present #1300 cases
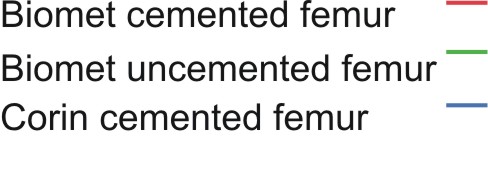
|
| 2 yrs | 5 yrs | 10 yrs |
| Group 1: Corin cemented femur | 96.8% | 95.9% | 92.4% |
| Group 2: Biomet cemented femur | 98.0% | 97.5% | NA |
| Group 3: Biomet uncemented femur | 99.0% | NA | NA |
| Entire Group | 98.3% | 97.6% | 94.3% |
Results can be improved by preselecting for certain subsets of patients who are known to be better candidates. The results above, however, were achieved in a relatively unselected group of patients. My criteria for hip resurfacing are relatively broad; men and women up to age 65 with any type of hip arthritis who have not lost more than 1/3 of their femoral head due to the arthritic process.
In all patients signed up for uncemented hip resurfacing, a tight initial press-fit was achieved. In no cases did we abandon uncemented fixation and have to rely on cement. In no cases did we decide to convert to a stemmed total hip at the time of surgery.
These are my updated most recent results with hip resurfacing. The success rate is much higher than most series of hip resurfacing or stemmed total hip replacement. As with any implant system, increasing failures will occur as we follow patients longer. Late failures that we may expect are loosening of components or adverse wear problems. Late failures due to loosening of uncemented implants has been rare in past studies of uncemented stemmed total hips, therefore we are hopeful that the early results with this uncemented hip resurfacing will remain durable.
The Biomet Magnum and Recap components are FDA approved. Their use together as a total hip resurfacing combination is not FDA approved. This combination is approved for use in most other countries in the world. When a US surgeon decides to use them together this is defined as an off-label use. The FDA role is to regulate how implant companies market their devices in the US market; they are not empowered to regulate surgeon practice. Therefore Biomet may not promote off-label use, but surgeons are free to use their best judgment in treating patients.
As financial advisors like to say, past results do not guarantee future success. I have reviewed the most common complications that have or can be expected to occur. Of course, biological systems, such as the human body are extremely complex and sometimes react unexpectedly despite our best efforts and intentions. Therefore the problems listed above cannot be assumed to be the only complications that might occur. I am happy to answer any individual questions that you have about your special case. Most importantly, retaining the most skilled and experienced surgeon that you can find will maximize your chance of an excellent result. All other factors are secondary. I encourage you to compare results.
Thomas P. Gross, MD 1/11/2011
Thomas P. Gross, M.D.
Current status of uncemented femoral components in hip resurfacing.
January, 2010.
Uncemented femoral components for metal on metal total hip resurfacing have shown excellent results during the initial 3 years that I have been using this new technology. The early results that I have achieved in 0ver 800 cases since March 2007 are equivalent to the early results that I achieved with the same brand cemented femoral component.
Uncemented fixation of implants to bone is a proven technology that has generally surpassed the durability of cemented fixation to bone in traditional hip replacement surgery. In the long term (at 10 years) a higher percentage of hip implants using uncemented fixation still remain attached to the bone than cemented implants, especially in younger more active patients.
Fixation of total hip implants to bone can be accomplished by cement or by porous ingrowth technology (uncemented). Cement fixation is immediate. Cement is an acrylic material (methylmethacrylate) that is very brittle and also fairly toxic to bone cells. Cemented implants gradually loosen from the bone over time by reaction to the cement itself and due to gradual fatigue failure of this material. This process is faster in more active patients and faster in implant situations where the cement is stressed by shear forces rather than by compression forces.
Uncemented components are initially held to the bone by a very tight press-fit which is achieved by accurately preparing the bone so that the implant can be tightly hammered-on. The implants are so tightly wedged–on that the patient can bear full weight on them immediately. They do require a period of six to twelve months of bone ingrowth before they are considered well fixed. There is usually a small chance of failure of this bone ingrowth process in uncemented implants (<1%). But if ingrowth occurs, it is much more durable than cemented fixation and rarely fails in the long term.
Because orthopedic surgeons in
In hip resurfacing there is universal agreement that uncemented fixation is superior for the acetabular component. However, until recently, uncemented femoral components have not been available, therefore most hip resurfacing operations in the past have employed cemented fixation of the femoral component.
At the time that I began hip resurfacing in 1999, there was not yet general agreement that uncemented fixation was superior to cement in hip replacements. However, the evidence was mounting that uncemented fixation was better. I therefore did not think it was logical to use cemented fixation in hip resurfacing, an operation developed specifically with the more active younger patient in mind. The only companies pursuing hip resurfacing at the time were two small English companies: Corin and Midland Medical Technology (maker of the
I therefore worked with Biomet on an uncemented femoral component and the precision instrumentation required for this implant for five years. I first began implanting it in March 2007. The Biomet component has a full coating of Titanium plasma spray under the entire under-surface of the femoral component. Recently we have added an additional layer of hydroxylappatite (HA) to increase the speed and extent of bone ingrowth. This is the best implant available to maximize the chance of bone ingrowth. When I started working with Biomet to develop an uncemented femoral component, Corin also started to work on one. They were able to bring it to market in
Theoretically, cement is the weak link when long-term (> 10 years) fixation of the femoral component is contemplated. If uncemented femoral components can be shown to achieve reliably high rates of ingrowth in the short term, they will probably outperform cemented femoral components in the long-term.
At this point with nearly 2-year follow-up data on a matched group of patients, I see no difference in results whether cement or uncemented fixation is used. At this point we can be fairly certain that bone ingrowth has occurred in these components. Except for two cases where osteonecrosis occurred in the femoral head at 1 year, we have had no failures of bone ingrowth in 430 patients that have are at least one year postop, and 157 that are at least two years postop.
COMPARISON STUDY
Uncemented Group Cemented Group
Number 191 96
Avg. Follow-up 2 years 2 years
Harris Score 94+ 10 96+ 6
UCLA Activity 8 + 2 7 + 2
Failures 2% 2%
SURVIVORSHIP CURVES
Total 191 cases
In summary:
- Uncemented femoral resurfacing components are now available from BIOMET for any patient who desires them.
- No other companies are yet selling these in the US
- Corin has had an uncemented femoral component available in Europe for several years.
- At 2 years of follow-up there is no difference in the failure rate between cemented or uncemented femoral component.
- Uncemented fixation of implants is more durable at 10 years than cement in hip replacement surgery especially in young active patients.
- Most clinical data on hip surface replacement to date is based on an uncemented acetabular component and a cemented femoral component.
- I now use uncemented components on virtually all hip resurfacing operations, unless the patient specifically requests the cemented femoral device.
- Thomas P. Gross, MD January, 2010
