What is a Femoral Osteotomy?
Proximal femoral osteotomy is currently commonly used for adults in the treatment of hip fracture nonunions and malunions and in cases of congenital and acquired hip deformities.
History of the Procedure
Proximal femoral osteotomy was a technique used in adults in the early part of the 20th century for the treatment of hip dysplasia and osteoarthritis. Varus- and valgus-producing osteotomies were aimed at maximizing joint congruity and redistributing the weightbearing load across the femoral head to a less affected area. Historically, the best results were obtained in patients with long-standing deformities, including Perthes osteonecrosis, coxa vara, and developmental dysplasia.
 Modern periacetabular osteotomies and joint arthroplasty techniques have narrowed the indications for this once common procedure. Proximal femoral osteotomy continues to find application in adults for the treatment of hip fracture nonunions and malunions and in cases of congenital and acquired hip deformities.
Modern periacetabular osteotomies and joint arthroplasty techniques have narrowed the indications for this once common procedure. Proximal femoral osteotomy continues to find application in adults for the treatment of hip fracture nonunions and malunions and in cases of congenital and acquired hip deformities.
Problem
In young patients with symptomatic hip disease, total joint arthroplasty has traditionally been a suboptimal solution. Problems with accelerated bearing wear and premature implant loosening leading to early revision surgery are well documented in this patient population. Intertrochanteric osteotomy has some use in providing temporary relief of pain in this challenging group of patients. While newer bearing materials with improved wear properties may improve the longevity of total joints in young patients, data to support this position are yet lacking.
Patients with deformity of the proximal femur typically develop arthritis over time due to abnormal joint wear from malalignment. Deformities typically include a varus or valgus neck-shaft angle, rotational malalignments, and leg-length discrepancy in any combination. These deformities can be acquired, as in the case of proximal femur fracture malunions and nonunions, or developmental, as in the cases of fibrous dysplasia, coxa vara, and developmental dysplasia.
Regardless of the etiology, these patients with femoral deformity are at an increased risk for the development of pain and arthritis in the affected hip. Once arthritis has begun, the problem is further aggravated by the mechanical malalignment from the femoral deformity. Standard hip replacement techniques and prostheses are usually unsuitable for deformed proximal femora, thus increasing the complexity of the procedure, surgical risks, and possibly the longevity of the reconstructed joint.
The benefits of early proximal femoral osteotomy to correctdeformity are two-fold. One, in the deformed hip prior to the onset of arthritic changes, the realignment often reduces symptoms, prevents further joint degeneration. In the deformed hip with arthritic changes, restoration of normal alignment can often decreases pain and improves function. Moreover, if the relief of symptoms is incomplete and the patient later requires hip replacement surgery, then the arthroplasty procedure is simplified by restoration of the anatomy.
Frequency
Proximal femoral osteotomy is commonly used in the treatment of nonunions of hip fractures. Both femoral neck and intertrochanteric fracture nonunions respond positively to valgus-producing realignment osteotomies. Malunions of hip fractures, including intertrochanteric type and unreduced slipped capital femoral epiphysis (SCFE), are other common indications for osteotomy. Infrequently, proximal femoral osteotomy is performed in adults for the treatment of hip arthritis and osteonecrosis.
Pathophysiology
Femoral neck nonunion
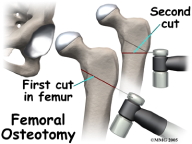
In femoral neck nonunion, the fracture fails to heal despite an adequate blood supply. Weightbearing forces across a vertically oriented fracture line produce shear stresses at the fracture site that favor the production of fibrous tissue. Valgus intertrochanteric osteotomy reorients the fracture site into a more horizontal position. Axial loading in this situation encourages osteogenesis and fracture union (see Images 1-3).
Intertrochanteric nonunion
Intertrochanteric hip fractures typically do not disturb the blood supply to the femoral head and tend to heal predictably. Nonunions of this common fracture pattern are usually the result of a combination of varus malalignment and inadequate stability of fixation. Treatment is aimed at correcting the varus neck-shaft angle to a neutral or slight valgus orientation and improving the stability at the fracture site often with a fixed-angle device (see Images 4-6).
Intertrochanteric malunion
When the fracture collapses into varus angulation and then goes on to bony union, a malunion results. The hallmark of this malunion is a varus neck-shaft angle with shortening of the ipsilateral femur, shortening of the abductor musculature or lever arm, and often trochanteric-pelvic abutment and a Trendelenburg gait with poor hip motion. This patient is at an increased risk for the development of hip arthritis. Intertrochanteric osteotomy serves to realign the hip joint, restore normal abductor mechanics, and reestablish equal leg lengths.
SCFE malunion
SCFE is a common fracture variant seen in the adolescent population. In many cases, in situ pinning of the displaced fracture is indicated, since this reduces the risk of osteonecrosis of the femoral head. If a displaced slipped epiphysis heals in situ, a fracture malunion can result. After remodeling, this malunion is characterized by coxa vara, femoral shortening, and retroversion of the femoral neck with a significant loss of hip motion. A valgus-producing proximal femoral osteotomy can correct the varus and reestablish normal rotation, both of which reorient the femoral head in the acetabulum, offering possible protection from the development of arthritis. This procedure also equalizes limb length and abductor tension, thereby normalizing gait.
Fibrous dysplasia
A shepherd's crook deformity of the proximal femur has long been associated with fibrous dysplasia. Repeated microfractures of the femoral neck lead to progressive displacement and healing of the femur in varus. Significant shortening of the femur, trochanteric-pelvic abutment, and shortening of the abductor lever arm occur concomitantly. Rotational deformity may also be present.
Patients report limb shortening, hip stiffness, and an inability to abduct the lower extremity, which can be particularly troublesome for women of childbearing age. Pain may be present as well. These patients are at risk for progression of the deformity, fracture of the femoral neck, and joint degeneration. Valgus-producing proximal femoral osteotomy serves to prevent progression of the deformity and the development of a fracture, reestablish a more normal femoral head–acetabular relationship, lengthen the extremity, tension the abductors, and greatly improve hip abduction.
Developmental dysplasia of the hip
Adults with hip dysplasia often have both acetabular and femoral deformity. The femoral neck assumes a valgus and anteverted orientation, while the acetabulum is shallow with varying degrees of uncovering of the femoral head, ranging from mild to subluxed to a frank dislocation. In select patients, surgery is indicated to improve femoral head coverage or better reduce the hip joint. A varus-producing proximal femoral osteotomy with derotation of the anteverted neck improves femoral head orientation. Often, this is combined with a periacetabular osteotomy to improve superolateral and anterior head coverage.
Osteoarthritis and osteonecrosis
The goal of the femoral osteotomy procedure is to alter the contact point across the articular cartilage during weight bearing. When arthritic change occurs without deformity, then a valgus-extension osteotomy moves the contact point of weight bearing forces to a new location on the femoral head, alleviating the pressure across the degenerated area of articular cartilage. This area of damaged cartilage has been shown to undergo a reparative process through which new collagen is created (see Images 7-8).
Clinical
Adults present with deformity about the hip from any number of etiologies, including hip fracture nonunion or malunion including SCFE, congenital coxa vara, shepherd's crook deformity from fibrous dysplasia, excessive femoral anteversion, developmental dysplasia of the hip, congenital or acquired femoral shortening, and soft tissue contractures about the hip.
A thorough examination is crucial before undertaking any osteotomy procedure to correct a deformity, as deformities commonly lie in multiple planes. Hip, knee, and ankle are examined, looking for deformity and joint range of motion. Hip joint contractures may be resolved through the osteotomy. Rotational profile of the lower extremity, including hip internal and external rotation and thigh foot axis, is documented. Limb length discrepancy is measured using blocks and later with radiographs.
Previous incisions, skin quality, and any signs of previous sepsis should be carefully sought.
Updated December 2008
